Costly Efficiencies
Healthcare Spending, COVID-19, and the Public/Private Healthcare Debate
CHRIS MOURÉ
May 2022
Abstract
Proponents of private healthcare often claim that the private sector is more ‘efficient’ at delivering healthcare services. This paper tests the privatization thesis in the context of the COVID-19 pandemic. Using a large sample of countries, I investigate how healthcare privatization affects the correlation between COVID-19 death rates and healthcare spending (as a share of GDP). In countries with healthcare that is mostly public, I find no correlation. However, in countries with significant healthcare privatization, I find that greater healthcare spending was associated with more COVID-19 deaths. This result is consistent with the theory of ‘capital as power’, which argues that to earn profits, the private sector seeks to strategically limit the provision of social goods.
Keywords
capital as power, COVID-19, healthcare spending, private healthcare, profit, public healthcare
Citation
Mouré, Chris. 2022. ‘Costly Efficiencies: Healthcare Spending, COVID-19, and the Public/Private Healthcare Debate’. Review of Capital as Power, Vol. 2, No. 2, pp. 17–45.
1 Public vs. private healthcare
THE debate over public versus private healthcare often turns on cost — particularly on how to reduce government spending. Proponents of private healthcare claim that the private sector is more ‘efficient’ and more ‘innovative’ than government, meaning it will deliver better results at a lower cost.1
This ‘privatization thesis’ is difficult to assess for two reasons. First, healthcare is typically delivered through a complex collaboration between public and private actors, making it hard to quantify the level of healthcare privatization. Second, countries face diverse public health challenges, making international outcomes hard to compare. Although the degree of healthcare privatization remains difficult to measure, the COVID-19 pandemic represents a unique opportunity to solve the second problem. The global nature of the pandemic meant that nearly every country experienced the same public health crisis at the same time. As such, the pandemic offers a rare occasion for testing the privatization thesis.2
This paper investigates how the level of healthcare privatization affected COVID-19 outcomes. Specifically, I measure the correlation between healthcare spending (as share of GDP) and COVID-19 death rates. I treat this correlation as a holistic measure of healthcare ‘efficiency’ — it measures the ability to convert dollars spent into lives saved.
Interestingly, I find that this correlation is clearly affected by the degree of healthcare privatization. In countries with healthcare that is largely public, there is no clear connection between healthcare spending and COVID-19 deaths (per capita). However, in countries with healthcare that is more privatized, I find that greater healthcare spending is associated with more COVID-19 deaths (per capita).
This evidence contradicts the privatization thesis. When it comes to the COVID-19 pandemic, privatized healthcare did not lead to better outcomes. Instead, private ‘efficiencies’ (if they exist) came at the cost of public health. From the perspective of mainstream economics, this outcome makes little sense. However, it is consistent with the theory of ‘capital as power,’ which argues that private-sector profits are realized not through ‘productivity,’ but through the strategic limitation of human activity.
The remainder of the paper is organized as follows. Section 2 reviews two opposing theories of the private sector. Neoclassical economics treats market activity as inherently productive. In contrast, the theory of capital as power argues that businesses earn profits through a process of ‘strategic sabotage.’ In Section 3, I apply the theory of capital as power to healthcare. I look for qualitative evidence that private healthcare providers seek to strategically limit services. After reviewing difficulties with the quantitative study of healthcare (Section 4), I investigate how healthcare privatization has affected COVID-19 outcomes (Section 5). Because this analysis is preliminary, I conclude by discussing remaining questions and avenues for future research (Sections 6 and 7).
2 The business of health
To understand the debate over healthcare privatization, one must start with economic theory. The idea that the private sector is more ‘efficient’ than government comes from neoclassical economics — the dominant school of economic thought. In marked contrast to neoclassical economics, the theory of ‘capital as power’ proposes that the private sector realizes profits through ‘strategic sabotage.’ In what follows, I briefly review these opposing theories.
2.1 The neoclassical view
According to neoclassical economics, markets are more ‘efficient’ at allocating resources than are governments. The idea is that because private firms must compete, they are driven to increase efficiency and lower costs (Rosenthal and Newbrander 1996, 207-208). Unlike private firms, governments lack competition, meaning they are essentially monopolies. As such, economists argue that governments have little incentive to lower costs or seek efficiencies (Gerdtham, Søgaard, Andersson, and Jönsson 1992, 6).
Summarizing the neoclassical view of healthcare, economists James Capretta and Kevin Dayaratna write:
[A] market-driven health system would work as one would expect it to — driving out waste and inefficiency and rewarding high quality and lower costs with greater market share.
(Capretta and Dayaratna 2013)
Neoclassical economists offer similar arguments on the ‘consumer’ side of healthcare. If consumers were forced to pay more for healthcare, economists reason, they ought to ‘consume’ healthcare services more efficiently. Thus, Kathryn Nix and Alyene Senger argue that US healthcare costs are high because users “are insulated from the cost of healthcare” (2012). Similarly, Capretta and Dayaratna argue that when healthcare is free, consumers use “more care than they [need]” (2013). But when users pay for healthcare services, they tend to avoid unnecessary costs.3
To summarize, neoclassical economists argue that private healthcare is superior to public healthcare for two main reasons:
-
The quest for profit leads private firms to become more efficient, leading to better healthcare outcomes.
-
When individuals pay directly for healthcare, they ‘consume’ these services more carefully.
If this worldview is true, then private healthcare should tend to minimize waste. And if healthcare spending does increase, it is because better services are being provided.
2.2 Capital is power
In contrast to neoclassical economics, Jonathan Nitzan and Shimshon Bichler’s theory of ‘capital as power’ sees private-sector profit as antagonistic to society. Building on the insights of the early twentieth century sociologist Thorstein Veblen, Nitzan and Bichler argue that business profits are realized not by ‘adding value,’ but through the strategic limitation (or ‘sabotage’) of industrial capacity and human wellbeing (2009, 233-235).
The goal of business, Nitzan and Bichler propose, is to sabotage society to just the right degree — enough to earn profits, but not so much that earnings decline and the economy stagnates. In Veblen’s words, business aims to charge “what the traffic will bear” (1908, 107). Since a return on investment is considered ‘normal’ in capitalist societies, the associated social sabotage becomes largely invisible — a mundane ‘cost of doing business’ (Nitzan and Bichler 2009, 242).
Nitzan and Bichler argue that strategic sabotage takes two main forms. First, business attempts to redirect industry toward ends that are more profitable. For instance, in healthcare, pharmaceutical companies often develop expensive drugs that are marketed to the rich, rather than developing (less profitable) drugs that could improve the health of the poor. Similarly, private hospitals tend to invest less in essential services (like emergency rooms), and instead spend money on expensive specialized procedures.
Second, Nitzan and Bichler argue that sabotage is visible as the systematic under-utilization of capacity. On that front, private hospitals tend to provide fewer hospital beds than their public counterparts (Buzelli and Boyce 2021). In other words, choking the market for hospital beds may be good way to earn a profit.
3 The strategic limitation of healthcare: qualitative evidence
According to the theory of capital as power, private healthcare realizes profits through strategic sabotage. In this section, I review evidence for the limitation of healthcare services in the context of the COVID-19 pandemic.
3.1 Private healthcare in Italy
I begin with the example of Italy. Over the last few decades, Italy attempted to cut costs by privatizing many elements of its national health service. In a recent paper, Maria Luisa Buzelli and Tammy Boyce argue that this privatization made the country “more vulnerable and unprepared to tackle the COVID-19 pandemic” (2021, 501). Their reasoning is simple: privatization led to a reduction in public health services, and these services are a key tool for mitigating the pandemic. Buzelli and Boyce note that in Italy, private hospitals provide a “limited range of services compared to public hospitals.”4 By focusing on specialized procedures, firms can charge a premium and so “ensure the private sector high returns” (2021, 502).
In the context of the COVID-19 pandemic, the Italian region of Lombardy provides a salient case study of the effects of healthcare privatization. Having invested heavily in specialized private medical care, the region found itself with only 0.74 primary care physicians per 1000 residents — about half the number found in France and Germany (Plagg et al. 2021, 3988). And while the region of Lombardy boasts the highest per capita income in Italy, during the early months of the pandemic the region had excess mortality rates that were five times higher than in neighboring Veneto (Varella 2021; Plagg 2021, 3988).
Tellingly, Buzelli and Boyce note that despite extensive privatization, public hospitals still provide “almost all emergency care in Italy” (502). So in many ways, private-sector investment has actually increased the burden on public hospitals. For example, public emergency rooms frequently get used for non-urgent care, largely because they provide their services for free (Plagg 2021).
Compared to public hospitals, it seems that private hospitals invest less in basic care. In Lombardy, private hospitals outnumber public hospitals, yet provide three times fewer hospital beds. And in Italy as a whole, there are roughly equal numbers of public and private hospitals. Yet private hospitals provide about 100,000 fewer beds (Buzelli and Boyce, 2021).
If the theory of capital as power is correct, this under-investment in hospital beds may indicate intentional limitation — a private-sector strategy for boosting profits.
3.2 Private healthcare in India
Like Italy, India relies heavily on private healthcare. In India, there are twice as many private hospitals as public ones. Furthermore, about 80% of the population lacks health insurance. And although public healthcare is provided for free, the system is underfunded and often delivers poor-quality care. This under-investment, Kamala Thiagarajan observes, “drive desperate patients towards private care” (2020, 1).
During the pandemic, private hospitals behaved poorly. According to Thiagarajan, private hospitals resisted government efforts to cap prices for COVID-19 treatment, and refused to offer free or subsidized services. Commenting on the widespread failure of Indian private healthcare, Owain Williams writes:
India has been particularly plagued by private hospitals refusing treatment as the public hospital systems in many states have been overrun. Patients have died, sometimes outside hospital doors, after failing to gain admission to multiple hospitals.
(Williams 2020, 3)
Faced with this crisis, Indian officials took emergency actions, including sequestering private hospitals, forcing them to stay open, and prosecuting clinics that refused to comply. But despite this effort, Williams reports that private hospitals were still “routinely breaching price caps and gouging, turning away COVID patients and hoarding beds” (2020, 3).
3.3 Healthcare sabotage?
In the face of private-sector failure during the pandemic, organizations like the World Bank and the World Health Organization (WHO) have tended to blame the pandemic itself. The idea is that the pandemic is a rare event that could not have been planned for. The possibility that private hospitals intentionally limit services (and therefore exacerbate the pandemic) borders on unspeakable (Hellowell 2020).
Some analysts see the reverse problem, claiming government is limiting the private sector’s pandemic response. For example, a recent WHO memo discusses ways that government can get in the way. “Emergency legislation, compounded by weak health systems and regulation,” the authors claim, “can limit the private sector’s role [in responding to the pandemic]” (WHO 2020, 3). Conveniently, this memo ignores the fact that in many countries (India, Malaysia, the Philippines, Indonesia, Thailand, Egypt), emergency legislation greatly expanded the private sector’s role, often by legally forcing firms to provide emergency services (Williams 2020, 3).
Although the nefarious behavior of private healthcare providers has shocked many pandemic commentators, it is unsurprising when viewed through the lens of capital as power. In developing the theory, Nitzan and Bichler observe that ‘stagflation’ (inflation combined with reduced industrial capacity) is a general feature of capitalist crises (2009, 378). In this light, private hospitals may simply have kept to the normal business playbook, attempting to profit from the crisis by raising prices and limiting services.
4 Quantifying healthcare
The qualitative evidence reviewed above paints an unflattering picture of private healthcare’s response to COVID-19. However, one can always counter that the stories have been ‘cherry picked,’ and so do not represent the wider pandemic experience. It is only by gathering widespread, quantitative evidence that we can cast judgement on the private-sector’s healthcare performance.
In Section 5, I look for quantitative evidence that healthcare privatization has affected pandemic outcomes. Before turning to this evidence, however, I discuss previous efforts to quantify the efficacy of public and private healthcare.
4.1 Measuring healthcare efficiency and quality
Studies that quantitatively compare public and private healthcare often focus narrowly on either the ‘quality’ of care, or its ‘efficiency.’ Rarely do such studies address the connections between cost efficiency and broader health outcomes.
A common problem is that studies of healthcare quality focus on a particular setting or type of service. But such narrow measures of quality have little bearing on the health of an entire society. For instance, private hospitals might provide superior care relative to their public counterparts. However, private hospitals exclude patients who cannot afford their services. If we are to evaluate private healthcare as a whole, we must include not just the care itself, but also the adverse effects of healthcare exclusion.
If we do not measure these exclusionary effects, we may draw dubious conclusions. Here is an example. In a meta-analysis of 80 studies, Berendes et al. (2011) looked at drug ‘availability’ within low-income and middle-income countries. They found that private-sector providers scored substantially higher than their public-sector counterparts. However, Berendes did not consider the fact that private clinics provide drugs only to those can afford them. So if one has sufficient funds, a private clinic might be superior to a public one. But if one lacks the necessary funds, then the private clinics’ drugs are effectively unavailable (regardless of what is on the shelves). In this case, we must balance on-the-shelf availability with the drug exclusion caused by privatization — something that Berendes fails to do.
Studies that measure ‘efficiency’ have similar flaws. Oddly, they do not connect ‘efficiency’ (i.e. cost reductions) to better health. For example, a popular way to measure ‘efficiency’ is to take a specific healthcare provider and calculate its ratio of ‘inputs’ to ‘outputs’ (Tiemann and Schreyögg 2009). (Inputs refer to costs like labour and supplies. Output refers to things like the number of patients served or the length of patient stays.) Unfortunately, this kind of measure says little about the quality of care, and even less about actual health outcomes.
Tellingly, Tiemann and Schreyögg cite several studies which found that greater input-output efficiency was associated with higher inpatient mortality. In their own study, Tiemann and Schreyögg try to ‘avoid’ this issue by using average mortality rates (per hospital) to ‘adjust’ for variation in the quality of care. But by ‘controlling’ for quality of care, what Tiemann and Schreyögg are actually doing is removing it from their analysis. And so they detach the gains of cost-efficiency from any understanding of whether health outcomes are improved or impaired.
My goal here is to avoid the mistakes described above. In Section 5, I propose a measure of healthcare that combines both cost-efficiency and general health outcomes.
4.2 Measuring healthcare privatization
To determine how healthcare privatization affected pandemic outcomes, we must measure the level of privatization. This measurement is difficult, largely because the provision of healthcare is often tightly integrated between public and private sectors.
Basu et al. note that national healthcare systems include a diverse array of public and private actors, often with funding and organizational structures that are intermixed (2021, 2). This complexity makes a ‘public-private’ distinction far from straightforward. Complicating things further, many countries lack data that describes the public-private distribution of healthcare resources.
Acknowledging the difficulty of separating healthcare into public and private components, Mackintosh et al. (2016, 2) provide three possible metrics for determining healthcare composition:
-
Demand side: the extent of private finance within total healthcare expenditure.
-
Supply side: the scale of the private sector in healthcare, as indicated by its weight in the delivery of care.
-
Commercialization: the accessibility of the public sector, proxied by the extent to which public healthcare relies on fees.
Due to the restricted scope of this paper (and the limited availability of relevant data), I estimate healthcare composition using the first metric. I measure the share of private health spending in total domestic health expenditure.
Importantly, there is evidence that private spending is a reliable measure of healthcare privatization. For instance, Basu et al. (2012, 9) note that a Chinese study found that healthcare privatization led to a significant increase in ‘out-of-pocket spending.’ (Out-of-pocket spending represents fees paid directly by healthcare users.) One worry is that out-of-pocket spending does not measure privatization, since some public healthcare systems also rely on user fees. (This is the case in Armenia.) However, public-sector fees rarely exist in isolation. More typically, they exist alongside a large private health sector (Torosyan, Romoniuk, and Krajewski-Suida 2007, 189).
Importantly, the World Bank provides data that can be used to distinguish between ‘out-of-pocket’ fees, and the remainder of private healthcare spending. For lack of a better word, I will call this remainder ‘non-out-of-pocket’ private spending. This non-out-of-pocket private spending likely captures the role of private insurance in financing healthcare. In the US, for instance, more than 80% of non-out-of-pocket private expenditure comes from private insurers (CMS Financial Report 2021, 2). More generally, different private healthcare organizations rely on different sources of funding. Mackintosh (2016) notes that private insurance typically funds large-scale healthcare providers, while out-of-pocket spending tends to fund smaller operations.
To summarize, it is difficult to rigorously measure the extent of healthcare privatization. However, the scale of private healthcare funding is likely a useful approximation. And any distinction between out-of-pocket and non-out-of-pocket spending may highlight the role of the private insurance industry.
4.3 Measuring COVID-19 outcomes
Like privatization, health outcomes can be difficult to measure. However, because I am focusing solely on the impact of the COVID-19 pandemic, outcomes become easier to measure. We simply count the number of COVID-related deaths (per capita). Fewer deaths is a better outcome. More deaths is a worse outcome.
Ignoring the problem of undercounting COVID-19 deaths (discussed in the Appendix), the bigger problem in this study is attributing death-rate differences to a particular cause. My goal here is to study the effects of healthcare privatization. But while healthcare is a major part of the pandemic response, it is not the only part. Many other factors can affect the severity of the pandemic, including social welfare provisions, government emergency responses, and cultural attitudes.
For example, it is no secret that the United States has had a particularly high COVID death toll. Nor is it a secret that the United States has a particularly privatized health sector. Still, analysts have largely ignored privatization as a factor that exacerbated the pandemic. Instead, they have focused on government policy failure (Altman 2020). Regardless of which assessment of the cause is ‘correct,’ the point is that it is difficult to isolate the effect of healthcare in mitigating the COVID-19 pandemic.
In the interests of exploratory research, this paper conducts a ‘single-factor’ analysis of COVID-19 outcomes as they relate to healthcare privatization. I do not attempt to ‘adjust’ for confounding factors. (I do, however, discuss possible confounders in Section 6.)
5 A quantitative study of healthcare composition, healthcare costs, and COVID-19 outcomes
The goal of this paper is to asses how public/private healthcare composition affected COVID-19 outcomes. My method involves two steps:
-
Sort countries into groups based on their level of healthcare privatization;
-
Measure the healthcare ‘efficiency’ of each group in relation to COVID-19 outcomes.
Step 1: Sort countries by healthcare privatization
I use four different metrics of healthcare privatization, described below. Each is based on the relative scale of private-sector finance in the provision of healthcare. Based on this scale, I divide countries into two groups — one in which the public sector dominates healthcare, and one in which the private sector is more dominant. The metrics are as follows:
-
Private healthcare spending as a share of total healthcare expenditure. This measure is a broad indicator of healthcare privatization. I differentiate between countries in which the private sector contributes less than 50% of total health spending, and countries in which the private sector contributes more than 50% of total health spending.
-
Out-of-pocket spending as a share of total healthcare expenditure. ‘Out-of-pocket’ spending consists of healthcare fees paid directly by patients. This measure captures how individuals fund private healthcare. I differentiate between countries in which out-of-pocket spending is greater than 50% of total healthcare expenditure, and countries in which it is less than 50% of expenditure.
-
Private non-out-of-pocket spending as a share of total healthcare expenditure. Non-out-of-pocket private spending consists mostly of the money spent by private insurance companies. I differentiate between countries in which private non-out-of-pocket spending is greater than 10% of total healthcare expenditure, and countries in which it is less than 10% of expenditure.
-
The ratio of private non-out-of-pocket spending to public spending. This measure compares the scale of the corporate healthcare sector to the public healthcare sector. I differentiate between countries in which private non-out-of-pocket spending is greater than 20% of public healthcare expenditure, and countries in which it is less than 20% of public expenditure.
Step 2: Measure COVID outcomes as a function of healthcare costs
After grouping countries using the categories above, I measure the severity of the COVID-19 pandemic as a function of healthcare costs. The idea is to connect health outcomes (COVID-19 deaths) with the cost of provisioning healthcare. If private healthcare is more ‘efficient’ than public healthcare (as advocates claim), then this efficiency ought to show up in COVID-19 outcomes.
To test this possibility, I take the two groups of countries (discussed above) and measure the correlation between cumulative COVID-19 deaths per capita and total healthcare spending as a share of GDP. (COVID-19 deaths are counted as of December 31, 2020. Healthcare spending is measured in 2018, the most recent year with available data.)
If healthcare is ‘efficient’ (at responding to pandemics), we expect that greater spending ought to lead to fewer COVID-19 deaths. Conversely, if healthcare spending is ‘wasteful,’ then greater spending could actually lead to more COVID-19 deaths.
5.1 Results
Pandemic outcomes sorted by private-sector health spending
I look first at how COVID-19 outcomes vary as a function of the private sector’s share of total health spending. Figure 1 shows the results. Each panel plots COVID-19 death rates against healthcare spending as a share of GDP. Panel A shows countries in which healthcare is dominated by the public sector. (These are countries in which private-sector spending is less than 50% of total healthcare expenditure.) Panel B shows countries in which healthcare is dominated by the private sector. (These are countries in which private-sector spending is greater than 50% of total healthcare expenditure.)
There is a clear distinction between the two types of countries. In countries where the public sector dominates total health spending (Fig. 1A), there is no significant relation between COVID-19 death rates and healthcare costs (measured as a share of GDP). However, in countries where the private sector dominates healthcare (Fig. 1B), there is a strong positive correlation between death rates and healthcare costs. In other words, in countries where healthcare is mostly private, greater healthcare spending was associated with more COVID-19 deaths.
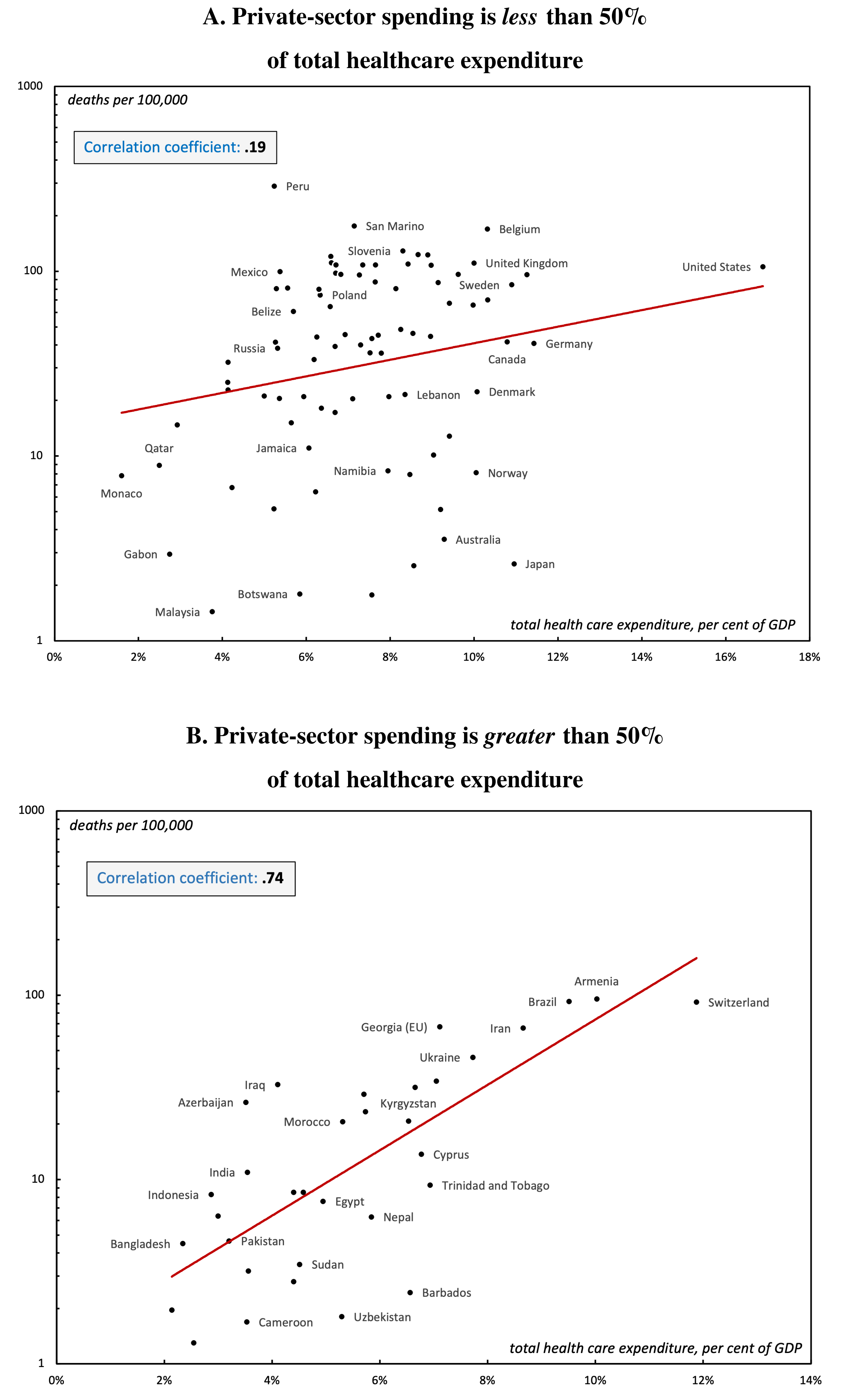 Figure 1: COVID-19 deaths vs. healthcare costs, differentiated by the private sector’s share of total healthcare expenditure.
Figure 1: COVID-19 deaths vs. healthcare costs, differentiated by the private sector’s share of total healthcare expenditure.
Note: Both panels show how COVID-19 death rates (vertical axis, log scale) relate to healthcare spending as a share of GDP (horizontal axis). Panel A contains countries in which the private sector contributes less than 50% of total healthcare spending. Panel B contains countries in which the private sector contributes greater than 50% of total healthcare spending. Death rates are measured as of December 31, 2020. Healthcare spending was measured in 2018. The red line indicates an exponential regression. Correlation is measured between healthcare spending and the log of COVID deaths. For data sources, see the Appendix.
Pandemic outcomes sorted by out-of-pocket health spending
Let’s now look at how COVID-19 outcomes vary as a function of out-of-pocket healthcare spending. This expenditure measures the fees that individuals pay to use healthcare services. (Note that these fees may be paid to both public and private healthcare providers.)
Figure 2 shows the results. Each panel plots COVID-19 death rates against healthcare spending as a share of GDP. Panel A shows countries in which out-of-pocket spending is less than 50% of total healthcare expenditure. Panel B shows countries in which out-of-pocket spending is greater than 50% of total healthcare expenditure.
We again find a distinction between the two types of countries. In countries where user fees contribute a minority of healthcare expenditure (Fig. 2A), there is weak relation between COVID-19 death rates and healthcare costs. However, in countries where healthcare is funded mostly by user fees (Fig. 2B) there is a positive correlation between death rates and healthcare costs.
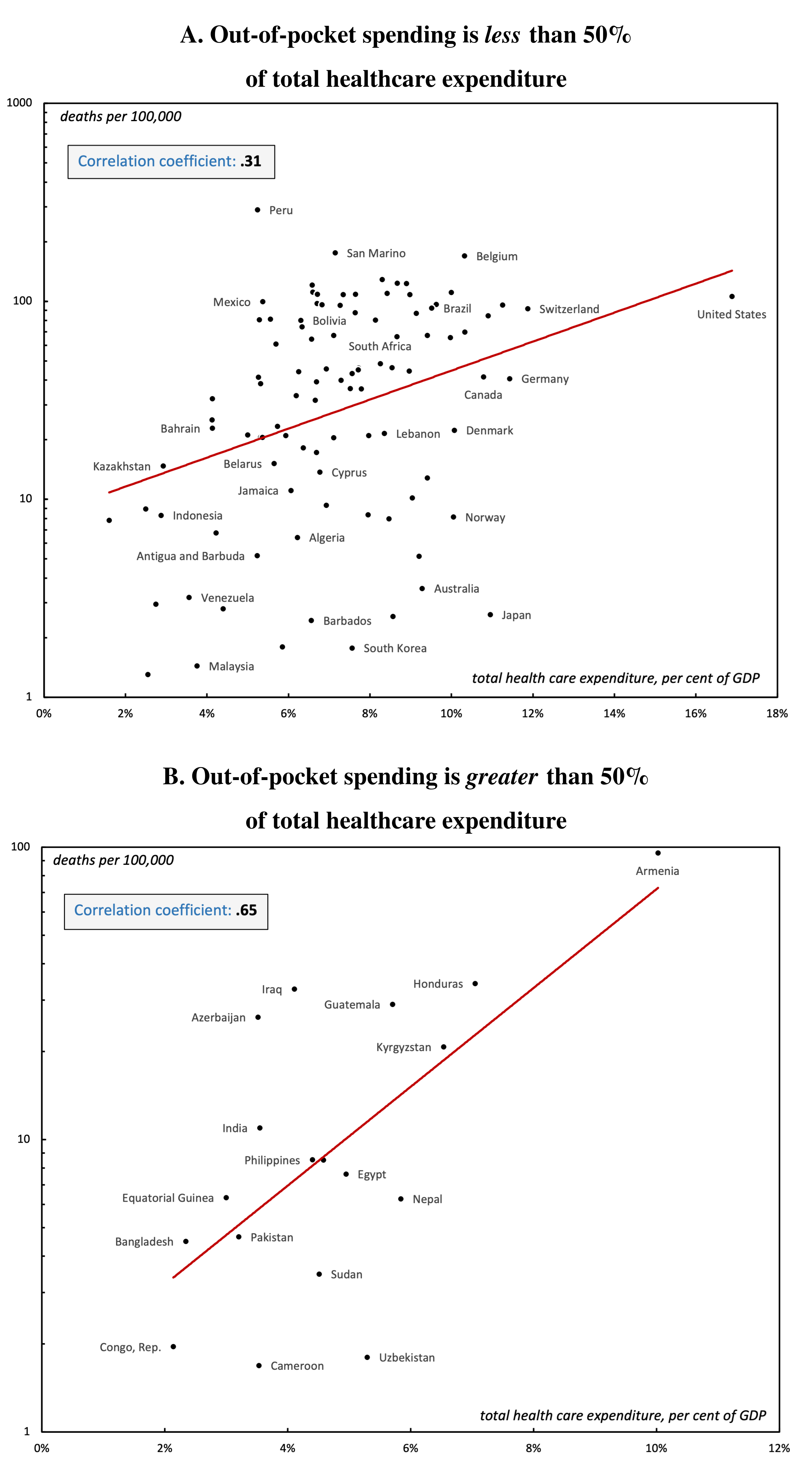 Figure 2: COVID-19 deaths vs. healthcare costs, differentiated by out-of-pocket spending as a share of total healthcare expenditure.
Figure 2: COVID-19 deaths vs. healthcare costs, differentiated by out-of-pocket spending as a share of total healthcare expenditure.
Note: Both panels show how COVID-19 death rates (vertical axis, log scale) relate to healthcare spending as a share of GDP (horizontal axis). Panel A contains countries in which private out-of-pocket spending is less than 50% of total healthcare spending. Panel B contains countries in which private out-of-pocket spending is greater than 50% of total healthcare spending. Death rates are measured as of December 31, 2020. Healthcare spending was measured in 2018. The red line indicates a exponential regression. Correlation is measured between healthcare spending and the log of COVID deaths. For data sources, see the Appendix.
Pandemic outcomes sorted by private non-out-of-pocket health spending
Finally, let’s look at how COVID-19 outcomes vary as a function of private non-out-of-pocket healthcare spending. Unlike out-of-pocket spending (user fees), non-out-of-pocket spending captures the role of private healthcare insurers. The greater this non-out-of-pocket spending, the more that healthcare is funded by private insurance companies.
Using the same convention as in the previous charts, Figure 3 differentiates COVID outcomes by private non-out-of-pocket spending as a share of total healthcare expenditure. Panel A shows countries in which private non-out-of-pocket spending is less than 10% of total healthcare expenditure. Panel B shows countries in which private non-out-of-pocket spending is greater than 10% of total healthcare expenditure.
Again, the two types of countries show different patterns. When the private insurance industry is small (Fig. 3A), there is a weak correlation between COVID-19 deaths and healthcare costs. However, when the private insurance industry is large (Fig. 3B), COVID-19 deaths increase with healthcare costs.
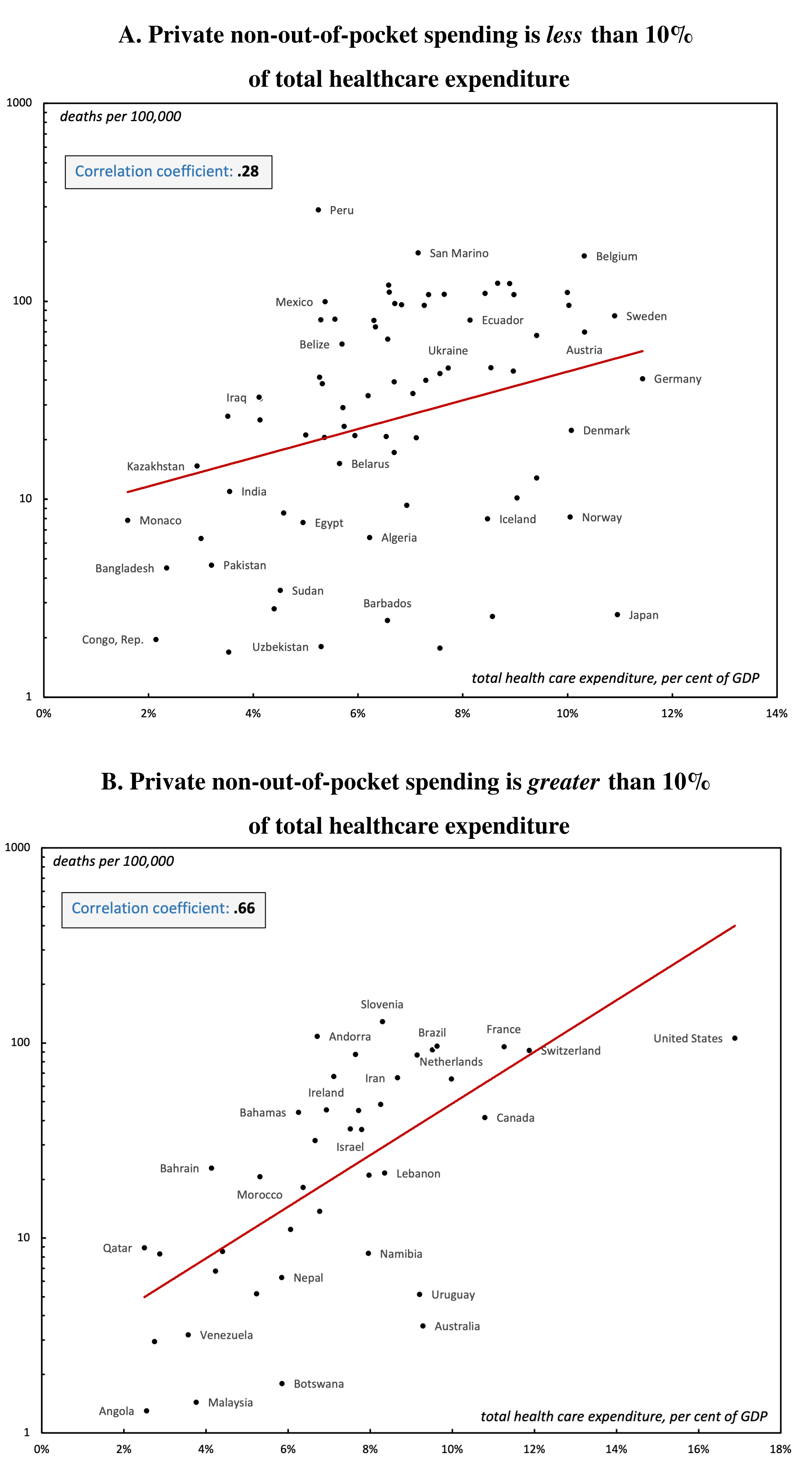 Figure 3: COVID-19 deaths vs. healthcare costs, differentiated by private non-out-of-pocket spending as a share of total healthcare expenditure.
Figure 3: COVID-19 deaths vs. healthcare costs, differentiated by private non-out-of-pocket spending as a share of total healthcare expenditure.
Note: Both panels show how COVID-19 death rates (vertical axis, log scale) relate to healthcare spending as a share of GDP (horizontal axis). Panel A contains countries in which private non-out-of-pocket spending is less than 10% of total healthcare spending. Panel B contains countries in which private non-out-of-pocket spending is greater than 10% of total healthcare spending. Death rates are measured as of December 31, 2020. Healthcare spending was measured in 2018. The red line indicates a exponential regression. Correlation is measured between healthcare spending and the log of COVID deaths. For data sources, see the Appendix.
Figure 4 shows an alternative way of gauging the size of private non-out-of-pocket spending. Instead of comparing this spending to total healthcare expenditure (as in Figure 3), I compare it to public healthcare expenditure. This comparison yields the strongest distinction in COVID-19 outcomes.
In countries where private non-out-of-pocket spending is less than 20% of the size of public health expenditure (Fig. 4A), there is no significant correlation between COVID-19 deaths and healthcare costs. However, when private non-out-of-pocket spending is greater than 20% of the size of public health expenditure (Fig. 4B), there is a tight correlation between healthcare costs and COVID-19 deaths.
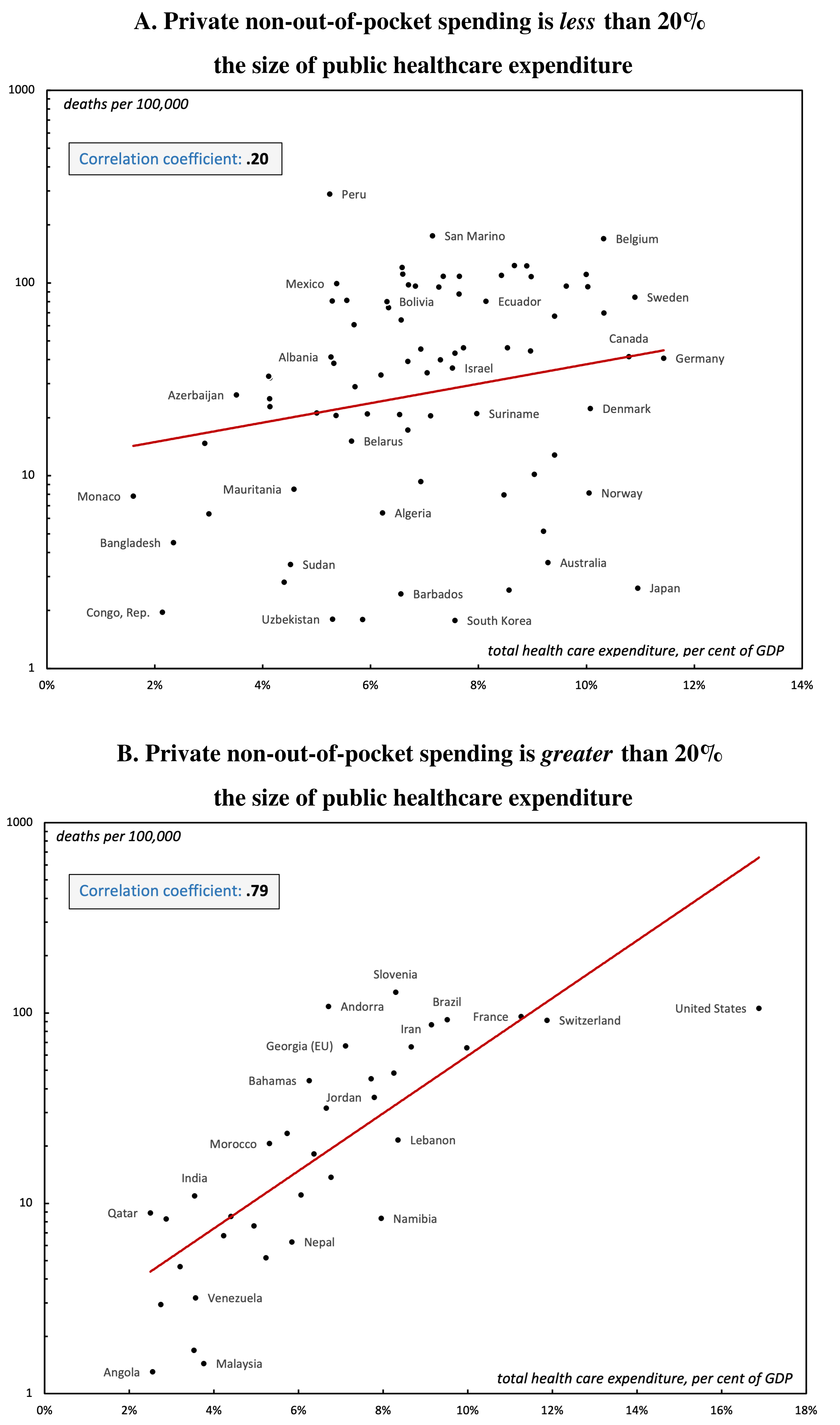 Figure 4: COVID-19 deaths vs. healthcare costs, differentiated by the size of private non-out-of-pocket spending relative to public healthcare expenditure.
Figure 4: COVID-19 deaths vs. healthcare costs, differentiated by the size of private non-out-of-pocket spending relative to public healthcare expenditure.
Note: Both panels show how COVID-19 death rates (vertical axis, log scale) relate to healthcare spending as a share of GDP (horizontal axis). Panel A contains countries in which private non-out-of-pocket spending is less than 20% of public healthcare spending. Panel B contains countries in which private non-out-of-pocket spending is greater than 20% of public healthcare spending. Death rates are measured as of December 31, 2020. Healthcare spending was measured in 2018. The red line indicates a exponential regression. Correlation is measured between healthcare spending and the log of COVID deaths. For data sources, see the Appendix.
5.2 Results summary
As a whole, the evidence suggests that healthcare privatization relates strongly to COVID-19 outcomes. Tables 1 and 2 summarize the results. Across my four measures of healthcare composition, I find a consistent distinction between countries with mostly public healthcare and countries with mostly private healthcare.
In countries where healthcare is largely public, COVID-19 death rates correlate weakly with healthcare costs, as shown in Table 1. In these countries, it seems that healthcare spending is not a major determinant of COVID-19 outcomes. However, in countries where healthcare is largely private, COVID-19 death rates correlate strongly with healthcare costs, as shown in Table 2. In these countries, it seems that greater healthcare spending led to worse pandemic outcomes.
| Sorting method | Correlation between COVID-19 deaths and healthcare costs as a share of GDP |
|---|---|
| Private sector spending is less than 50% of total healthcare expenditure | 0.19 |
| Out-of-pocket spending is less than 50% of total healthcare expenditure | 0.31 |
| Private non-out-of-pocket spending is less than 10% of total healthcare expenditure | 0.28 |
| Private non-out-of-pocket spending is less than 20% the size of public healthcare expenditure | 0.20 |
| Average | 0.25 |
| Sorting method | Correlation between COVID-19 deaths and healthcare costs as a share of GDP |
|---|---|
| Private sector spending is greater than 50% of total healthcare expenditure | 0.74 |
| Out-of-pocket spending is greater than 50% of total healthcare expenditure | 0.65 |
| Private non-out-of-pocket spending is greater than 10% of total healthcare expenditure | 0.66 |
| Private non-out-of-pocket spending is greater than 20% the size of public healthcare expenditure | 0.79 |
| Average | 0.71 |
6 Discussion
To understand the relation between privatized healthcare and COVID-19 outcomes, it is helpful to return to the opposing economic theories discussed in Section 2.
According to neoclassical economics, markets are the most ‘efficient’ way of allocating resources. The competition for profits is supposed to drive down prices and increase the quality of goods and services. Governments, in contrast, are characterized as ‘inefficient’ and ‘wasteful.’ By offering free and/or subsidized services, governments (economist claim) encourage consumers to use more than is necessary.
Nitzan and Bichler’s theory of ‘capital as power’ views things differently. It argues that the goal of private business often runs counter to the interests of society. Although capitalists may attribute profit to ‘efficiencies,’ Nitzan and Bichler argue that in broader terms, profit stems from ‘strategic sabotage.’ In other words, profit signals social ‘inefficiency.’ In normal times, this sabotage is consider a banal ‘cost of doing business.’ But during times of crisis, private-sector sabotage tends to become sharper and creates effects that are more severe.
In Section 3, I reviewed some of the qualitative effects of the private-sector sabotage of healthcare. In general, the private sector tends to invest in specialized (non-urgent) care, because that is what is most profitable. Relative to public healthcare, private hospitals provide less basic care and fewer emergency services. And when the private sector does provide basic services, they are available only to those who can afford them. It seems plausible that during a pandemic, this private-sector formula will perform poorly.
The quantitative evidence in Section 5 bears out this hypothesis. The results indicate a clear difference in COVID-19 outcomes between countries with mostly public healthcare and those with mostly private healthcare. In countries with mostly public healthcare, there was little relation between healthcare spending and COVID-19 deaths. However, in countries with mostly private healthcare, greater healthcare spending was associated with more deaths.
This finding makes little sense from the perspective of neoclassical economics. If the private sector is ‘efficient,’ then more healthcare spending ought to indicate ‘better’ healthcare. But at least when it comes to dealing with a pandemic, this idea seems to be false. Instead, spending on private healthcare was actually deleterious to public health. While paradoxical from a neoclassical perspective, the results are consistent with the theory of capital as power. It seems plausible that the private sector diverts healthcare investment to activities that are profitable, but not in the best interests of social health. By doing so, it leaves society more vulnerable to pandemics.
That said, the analysis in this paper is limited in scope, and therefore leaves many details for future research. Here are some questions to consider.
Why, for instance, is there no evidence that greater healthcare spending improves COVID-19 outcomes? In other words, among countries with pubic healthcare, why don’t we find a negative correlation between healthcare expenditure and COVID-19 death rates? An obvious answer is that no healthcare system (even highly public ones) is explicitly designed to deal with a pandemic. Instead, as health spending expands, it seems likely that societies tend to invest more in specialized treatments — treatments that are beneficial during normal times but superfluous during a pandemic. In this light, perhaps private healthcare simply exacerbates the specialization problem, funneling money away from basic care.
Another question: if we broadened the analysis to include many (possible) determinants of COVID-19 severity (other than healthcare privatization), what might we find? Here are three important factors to include in future research:
-
The age profile of the country. The mortality rate for COVID-19 is highly age-dependent, with lethality increasing significantly in older patients (Levin et. al. 2020). This suggests that COVID-19 deaths per capita may be higher in countries with older populations. Given that many wealthier countries in Europe have both high public healthcare spending and older populations, these demographics might affect the relation between COVID-19 deaths and healthcare spending.
-
Strength of non-healthcare policies used to mitigate the pandemic. During the pandemic, governments used a variety of policies to slow the spread of the virus, including lockdowns, border closures, stay-at-home orders, and mask-mandates. There have been several studies examining the link between these measures and health outcomes, with mixed results (see for instance Bjørnskov 2021; Bendavid et. al. 2021; Lau et. al. 2020). It is important to study how these measures affected mortality, and how these policies might relate to the public/private composition of healthcare. Did countries with stronger public healthcare tend to impose stronger non-healthcare measures? Did countries with weaker public healthcare systems tend to rely more heavily on non-healthcare government responses?
-
Resistance to public health measures. In many countries, governments struggled to get citizens to follow pandemic restrictions. This resistance was both individual and institutional. At the individual level, people chose to break curfews and stay-at-home orders, refused to close their businesses, and (later in the pandemic) refused to get vaccinated. At the institutional level, groups put pressure on governments to avoid lockdowns, delay business closures and border closures, and to not mandate vaccination. Given the business case for staying open, an interesting possibility is that the private sector in general (not just private healthcare) acted to worsen pandemic outcomes. If that is true, perhaps by measuring healthcare privatization, we are proxying the level of privatization in the society at large.
These three factors are but the tip of a long list of variables that might affect pandemic outcomes in co-relation with healthcare composition. Fortunately, the COVID-19 crisis is likely to be the most intensely studied pandemic in human history. So future researchers will not be short on data.
7 Conclusion
This study attempted to shed light on the longstanding debate over public vs. private healthcare. Because it is a major talking point for advocates of private healthcare, I focused on the issue of healthcare costs. Private healthcare proponents argue that public healthcare spending is ‘unsustainable,’ and that the private sector is the smarter choice for providing healthcare. I argued that because the COVID-19 pandemic affected every healthcare system in the world simultaneously, it provided a rare opportunity to test this claim.
The results show that in countries where the private sector plays a dominant role in funding healthcare, greater total health expenditure predicted worse COVID-19 outcomes. In contrast, among countries with healthcare that was mostly public, there was little correlation between healthcare spending and COVID-19 deaths. This finding contradicts the argument that private-sector healthcare is more ‘efficient’ (meaning it provides the same or better care at a lower price) than public healthcare. When it comes to pandemic outcomes, this was simply not true.
However, the evidence is consistent with the theory of ‘capital as power,’ which argues that private-sector profits are of negative social value — the result of strategic limitation and sabotage. Viewed through the lens of capital as power, the positive correlation between COVID- 19 deaths and healthcare expenditure may reflect two sides of the same process: the increasing control of business interests over a country’s healthcare system. As private control over healthcare increases, there is an increase in the level of ‘sabotage,’ and therefore a decrease in the quality of overall public health.
Having proposed a possible explanation for the evidence, I admit that this study is exploratory. It is based on a single-factor analysis, and therefore cannot capture the many determinants of public health. To aid future research, gathering information about the interaction between public and private healthcare should be a top priority for researchers, governments, and international organizations. There is also likely a need to better theorize the relationship between healthcare and the dynamics of capitalism.
While this paper is exploratory, the evidence suggest that in private healthcare, there is a conflict of interest between profit and public health. As the pandemic has tragically revealed, the cost of this conflict (whether counted in dollars or lives) is unsustainable.
Appendix
The data used in this paper is available at the Open Science Framework: https://osf.io/sb53k/
Alternative date for counting COVID-19 deaths
The results discussed in this paper are relatively robust to changes in the date when COVID-19 deaths are counted. To illustrate this fact, Tables 3 and 4 show the correlations found when summing COVID-19 deaths on September 19, 2021 (instead of December 31, 2020). There remains a clear distinction between countries with mostly public healthcare, and those with more privatized healthcare.
Table 3: COVID-19 outcomes in countries where the public sector dominates healthcare (alternative date for counting death rates)
| Sorting method | Correlation between COVID-19 deaths and healthcare costs as a share of GDP |
|---|---|
| Private sector spending is less than 50% of total healthcare expenditure | 0.09 |
| Out-of-pocket spending is less than 50% of total healthcare expenditure | 0.20 |
| Private non-out-of-pocket spending is less than 10% of total healthcare expenditure | 0.27 |
| Private non-out-of-pocket spending is less than 20% the size of public healthcare expenditure | 0.17 |
| Average | 0.18 |
Table 4: COVID-19 outcomes in countries where the private sector dominates healthcare (alternative date for counting death rates)
| Sorting method | Correlation between COVID-19 deaths and healthcare costs as a share of GDP |
|---|---|
| Private sector spending is greater than 50% of total healthcare expenditure | 0.71 |
| Out-of-pocket spending is greater than 50% of total healthcare expenditure | 0.63 |
| Private non-out-of-pocket spending is greater than 10% of total healthcare expenditure | 0.57 |
| Private non-out-of-pocket spending is greater than 20% the size of public healthcare expenditure | 0.74 |
| Average | 0.66 |
Data for COVID-19 death rates
COVID-19 data is from John Hopkins University, accessed via the 91-DIVOC Project.
I measured cumulative COVID-19 deaths as of December 31, 2020. This was mid-way through the first global peak of the pandemic. I chose this date because it was late enough that the pandemic had spread to a large number of countries, but still early enough that the data would accurately reflect the performance of the pre-existing healthcare system (i.e., before the system had been substantially affected by governments’ emergency funding).
I chose to use total death rates instead of ‘case-fatality rate’ (the other primary measure of COVID-19 impacts) for two reasons. First, while the case-fatality rate reflects one measure of the deadliness of the pandemic, the death count gives a broader sense of the severity of the outbreak. (If there are a large number of cases, a low case-fatality rate can obscure a large number of deaths.)
Second, because this study compares outcomes between countries, concerns about general downward bias in COVID reporting are less relevant. This is important, since one argument for using case-fatalities is that it mitigates bias. For instance, in their cross-country COVID-19 study, Ozkan et al. (2021, 2) prefer case-fatality to number of deaths because the measure “is [more] likely to moderate this bias given both the numerator and the denominator are likely to be lower than their true unobserved values.” Note, however, that this ‘moderation’ works only if both death and case counts are lower by a similar amount. In practice, there is no way to verify this moderation, since the degree of bias remains unknown. Assuming that most countries have a similar level of reporting bias, then the size of this bias is irrelevant for the present study.
Data for healthcare spending
Health expenditure data is from the World Bank. All data is from 2018, the most recent year available. Data series are as follows:
-
Total health expenditure as a % of GDP: series SH.XPD.CHEX.GD.ZS
-
Domestic private health expenditure as a % of total health expenditure: series SH.XPD.PVTD.CH.ZS
-
Out-of-pocket expenditure as a % of total health expenditure: series SH.XPD.OOPC.CH.ZS
I calculate non-out-of-pocket private expenditure by subtracting out-of-pocket expenditure from domestic private expenditure.
Data exclusion
I exclude countries that were missing either death rate data or health expenditure data. I also exclude countries in which more than 10% of health funding came from external (non-domestic) sources. External funding data comes from the World Bank, series SH.XPD.EHEX.CH.ZS.
Notes
Chris Mouré is a graduate student at York University. Email: cjmoure@yahoo.com
-
As an example of this attitude, a 2016 white paper from the Ontario Chamber of Commerce argues that Ontario’s healthcare system faces two main challenges. First, rising healthcare costs are being managed by ‘artificially limiting spending growth’ rather than by ‘increasing efficiency.’ Second, the health sector has ‘too few opportunities to bring their innovations to market’ (Challinor 2016, 5).↩︎
-
Although global pandemics are usually considered ‘rare,’ they may become more common in the future. Margaret Chan, former Director-General of the WHO, writes: “Population growth, incursion into previously uninhabited areas, rapid urbanization, intensive farming practices, environmental degradation, and the misuse of antimicrobials have disrupted the equilibrium of the microbial world.” The result is a situation in which “new diseases are emerging at the historically unprecedented rate of one per year” (WHO 2007, vi). Thus, the study of how differently organized healthcare systems have reacted to the COVID-19 pandemic is both timely and appropriate to the public/private healthcare debate.↩︎
-
Capretta and Dayaratna base their conclusions on a 1996 study by RAND economist Joseph Newhouse (Newhouse 1996).↩︎
-
According to Buzelli and Boyce, private healthcare providers focus on non-emergency care — things like “diagnostic procedures (e.g., laboratory tests), pharmaceuticals, specialist outpatient care, nonurgent interventions, residential care, and rehabilitation assistance” (2021, 502).↩︎
References
Altman, Drew. 2020. ‘Understanding the US Failure on coronavirus.’ British Medical Journal 370.
Basu, Sanjay, Jason Andrews, Sandeep Kishore, Rajesh Panjabi, and David Stuckler. 2012. ’Comparative Performance of Private and Public Healthcare systems in Low- and Middle-Income Countries: A Systemic Review. PLoS Medicine 9, no. 6.
Bendavid, E., Oh, C., Bhattacharya, J., & Ioannidis, J. 2021. ‘Assessing mandatory stay-at-home and business closure effects on the spread of COVID-19.’ European journal of clinical investigation 51, no. 4: e13484.
Berendes, Sima, Peter Heywood, Sandy Oliver, and Paul Garner. 2011. ’Quality of Private and Public Ambulatory Health Care in Low and Middle Income Countries: Systematic Review of Comparative Studies. PLoS Medicine 8, no. 4.
Bjørnskov, Christian. 2021. ‘Did Lockdown Work? An Economist’s Cross-Country Comparison.’ CESifo Economic Studies 67, no. 3 (September): 318–331.
Buzelli, Maria Luisa, and Tammy Boyce. 2021. ‘The Privatization of the Italian National Health System and its Impact on Health Emergency Preparedness and Response: The COVID-19 Case.’ International Journal of Health 51, no. 4: 501-508.
Capretta, James, and Kevin Dayaratna. 2013. ‘Compelling Evidence Makes the Case for a Market-Driven Health Care System.’ The Heritage Foundation. Accessed November 26, 2021. https://www.heritage.org/health-care-reform/report/compelling-evidence-makes-the-case-market-driven-health-care-system.
Centers for Medicare and Medicaid Services. 2021. CMS Financial Report for Fiscal Year 2021. https://www.cms.gov/files/document/cms-financial-report-fiscal-year-2021.pdf.
Challinor, Ashley. 2016. ‘Transformation through value and innovation.’ Ontario Chamber of Commerce. https://occ.ca/wp-content/uploads/HTI_March15-1.pdf
Fagen-Ulmschneider, Wade. 2021. 91-DIVOC Project. Accessed November 29. https://91-divoc.com/pages/covid-visualization/.
Gerdtham, Ulf, Jes Søgaard, Fredrik Andersson, and Bengt Jönsson. 1992. ‘An econometric analysis of health care expenditure: A cross-section study of the OECD countries.’ Journal of Health Economics 11, no. 1 (May): 63-84.
Hellowell, Mark. 2020. ‘Covid-19 and the collapse of the private health sector: a threat to countries’ response efforts and the future of health systems strengthening?’ Global Health Policy Unit. Accessed November 26, 2021. https://ghpu.sps.ed.ac.uk/covid-19-and-the-collapse-of-the-private-health-sector-a-threat-to-countries-response-efforts-and-the-future-of-health-systems-strengthening/.
Lau, H., Khosrawipour, V., Kocbach, P., Mikolajczyk, A., Schubert, J., Bania, J., & Khosrawipour, T. 2020. ‘The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China.’ Journal of travel medicine 27, no. 3: taaa037.
Levin, A. T., Hanage, W. P., Owusu-Boaitey, N., Cochran, K. B., Walsh, S. P., & Meyerowitz-Katz, G. 2020. ‘Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications.’ European journal of epidemiology 35, no. 12: 1123–1138.
Mackintosh, Maureen, Amoc Channon, Anup Karan, Sakthivel Selvaraj, Eleonora Cavagnero, and Hongwen Zhao. 2016. ‘What is the private sector? Understanding private provision in the health systems of low-income and middle-income countries.’ The Lancet 388, no. 10044 (August): 596-605.
Newhouse, Joseph. 1993. Free for all?: lessons from the RAND health insurance experiment. Harvard University Press.
Nitzan, Jonathan, and Shimshon Bichler. 2009. Capital as Power. A Study of Order and Creorder. RIPE Series in Global Political Economy. New York and London: Routledge.
Nix, Kathryn, and Alyene Senger. ‘The Promise of Consumer-Directed Health Plans: Studies Show Success at Reducing Costs and Maintaining Quality.’ The Heritage Foundation. Accessed November 26, 2021. https://www.heritage.org/node/12272/print-display.
Oksan, Aydin, Gulcin Oksan, Abdullah Yalaman, Yilmaz Yildiz. 2021. ‘Climate risk, culture and the Covid-19 mortality: A cross-country analysis.’ World Development 141 (January).
Plagg, Barbara, Guiliano Piccoliori, Jörg Oschmann, Adolf Engl, and Klaus Eisendle. ‘Primary Health Care and Hospital Management During COVID-19: Lessons from Lombardy.’ Risk Management and Healthcare Policy 14: 3987-3992.
Rosenthal, Gerald, and William Newbrander. 1996. ‘Public Policy and Private Sector Provision of Health Services.’ International Journal of Health Planning and Management 11, no. 3: 203-216.
Thiagarajan, Kamala. 2020. ‘Covid-19 exposes the high cost of India’s reliance on private healthcare.’ British Medical Journal 370 (September).
Tiemann, Oliver, and Jonas Schreyögg. 2009. ‘Effects of Ownership on Hospital Efficiency in Germany.’ Business Research; Göttingen 2, no. 2 (December): 115-145.
Torosyan, Arsen, Piotr Romaniuk, and Krzysztof Krajewski-Siuda. 2008. ‘The Armenian Healthcare System: Recent Changes and Challenges.’ Journal of Public Health 16, no. 3 (May): 183–90.
Varella, Simona. 2021. ‘Average annual gross salary in Italy in 2020, by region.’ Statista. Accessed November 29, 2021.
Veblen, Thorstein. 1908. On the Nature of Capital: Investment, Intangible Assets, and the Pecuniary Magnate. Quarterly Journal of Economics XXII (1, November): 104-136.
Williams, Owain David. 2020. ‘COVID-19 and Private Health: Market and Governance Failure.’ Development (Society for International Development) 63, no. 2-4: 181-190. http://dx.doi.org/10.1057/s41301-020-00273-x.
World Health Organization. 2007. ‘The World Health Report 2007: A Safer Future.’ https://www.who.int/publications/i/item/9789241563444.
World Health Organization. 2020. ‘Supporting private sector engagement during COVID019 – WHO’s approach.’ https://apo.who.int/publications/i/item/supporting-private-sector-engagement-during-covid-19-who-s-approach.